Heat Stroke FAQs for Parents
According to the CDC, heat illness during practice or competition is the leading cause of death among U.S. high school athletes.
Summer’s high temperatures put patients at increased risk for heat illness. There are several types of heat illness ranging in severity. Although heat illness can be fatal, death is preventable if quickly recognized and properly treated. Below are some Frequently Asked Questions that might help you and your child prepare for participation in the heat and avoid another catastrophic incident from occurring in our state.
Unfortunately, many schools in Arkansas are either not equipped to provide best practice care or have not coordinated with local emergency services to ensure they are equipped/able/educated in best practice care for Exertional Heat Stroke.
What is Exertional Heat stroke (EHS)?
Exertional heat stroke (EHS) is a medical emergency defined as life-threatening hyperthermia (core body temperature ≥ 40.5°C [105°F]) and central nervous system [CNS] dysfunction. EHS is one of the top three causes of sudden death in athletes. Early recognition and rapid cooling can reduce (or possibly even eliminate) both the morbidity and mortality associated with the organ damage that results from an extended time period of dangerous hyperthermia.
What are the signs and symptoms of heat cramps, heat exhaustion, heat stroke?
Heat illnesses are a spectrum of illnesses that occur due to heat exposure. This heat exposure can come from either environmental heat (air temperature) or simply intense exercise. These conditions can range from minor heat cramps to life-threatening heat stroke. Contrary to popular belief, heat illnesses do not exist on a continuum. You do not need to have heat cramps or syncope before you have heat exhaustion or suffer from heat stroke. The key determinant for good prognosis following a heat illness is rapid recognition and appropriate treatment. In the case of exertional heat stroke, delay in treatment nearly always leads to long term complications or death. Please use the following resources to learn more about signs and symptoms, treatment and returning to play following heat illness.
How can my child best prepare for participating in the heat?
While heat illness is not necessarily 100% preventable, there are many things one can do to help minimize the risk of suffering from a heat illness. Below is a list of things that you can do to prepare your body to participate in the heat.
Heat acclimatization: getting used to exercise and/or protective equipment in the heat is crucial personal protection against heat illness. In order for this to be effective, gradual onset of exercise duration and intensity takes place over the course of 10-14 days. In Arkansas, teams are required to facilitate heat acclimatization in August, but for only 5 days. It’s important for parents to know that full acclimatization takes longer than this. If your son/daughter has been exercising outdoors all summer, they are partially acclimatized.
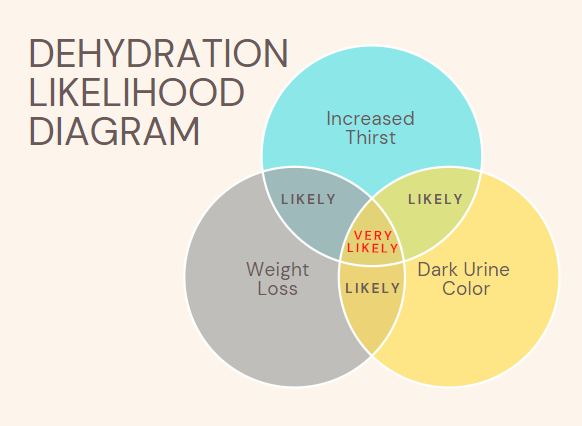
Hydration: Three main factors should be regarded as efficient self-checks for hydration each day.
Body weight: in order to properly recover, body weight should be back to what it was the day before prior to exercise in the heat. Weigh yourself every day upon waking up. If it’s low, you should have an extra drink before working out.
Urine color: a properly hydrated individual should have urine that looks like lemonade, not iced tea. If urine is darker, the person is likely dehydrated and should have an extra drink prior to exercise in the heat.
Thirst: internal thirst is a personal cue for hydration. If you are thirsty, you should try to quench your thirst prior to activity. While heat illness is not necessarily 100% preventable, there are many things one can do to help minimize the risk of suffering from a heat illness. Below is a list of things that you can do to prepare your body to participate in the heat.
The diagram below shows the relationship between these three factors.
Sleep: sleep is essential to athletic recovery and is a major focus at the higher levels of competition. Exertional heat stroke is more common in individuals who get <7 hours of sleep per night. Assure adequate sleep by fostering more than 7-8 hours of sleep consistently before exercise in the heat.
Illness: Current, or even recent, illness is associated with greater risk of heat illness. Anyone not feeling good, has gastrointestinal upset, or cold- or flu-like symptoms will achieve no gain from working out in the heat, and may actually prolong their illness. It is best for sick, or recently sick, athletes to take a day or 2 off from exercise in the heat prior to full return to participation.
Please use the following resources to learn more about what you can do to better prepare for participating in the heat.
What guidelines does Arkansas have in place that member schools must follow in regards to heat illness?
There are currently many guidelines, recommendations and laws that every AAA member school is expected to follow. Unfortunately it is up to the schools to ensure that all of these things are being done. There is no enforcement arm of the AAA that can or will enforce these things on the school. Below are items that ALL AAA member schools should be doing.
The Arkansas Activities Association requires schools to be using a WBGT assessment of environmental conditions and utilize a policy for activity/equipment modifications fostering safe play in the heat.
The AAA handbook states that all football teams MUST have an annual parent meeting concerning heat illness.
State law requires that schools have accessible tubs for cold-water immersion if an exertional heat stroke were to occur during activity in the heat.
State law requires that schools have an appropriate emergency action plan for any emergencies that may arise during practices/games.
State law requires an automated external defibrillator is on-site when sanctioned activity takes place.
Schools should work with local EMS providers to ensure an efficient recognition and treatment for any emergency scenario, including exertional heat stroke.
Ensuring Heat Illness Safety in Schools
While Arkansas has guidelines for heat illness prevention, enforcement is lacking. Parents should proactively check if their child's school is following safety protocols. Here's a checklist of essential steps schools should take:
1. Preseason Parent Meeting: Mandatory for football, recommended for all outdoor sports. Covers hydration, risk factors, prevention, and emergency procedures.
2. Emergency Action Plans (EAP): Annual review and rehearsal with coaches and EMS to ensure quick response in emergencies.
3. WBGT Monitoring: Schools must use Wet Bulb Globe Temperature devices to assess heat stress and adjust practices accordingly.
4. Core Temperature Measurement: Only rectal temperatures are reliable for diagnosing Exertional Heat Stroke (EHS). Ensure trained professionals are available for this measurement.
5. Emergency Cold Tub Access: Immediate cold water immersion for athletes with core temperatures above 105°F is critical for survival. Schools must have a ready-to-use cold tub on site.
For more details, please refer to the Recognizing and Treating Heat Illnesses video on initial treatment for exertional heat stroke.
What questions should I be asking my school or organization to know if they are ready?
Does our school district have a Certified Athletic Trainer?
If not, why not?
Does our school district have heat specific policy and procedures?
Where can this policy be found?
Does it include all of the following?
Acclimatization?
WBGT?
Where is it located?
When is it taken?
How often?
Are practice AAA modifications followed?
Are readings and accommodations recorded?
Core temp assessment?
Does our school have the necessary equipment?
If not, then who will perform this and when?
Has this been discussed and coordinated with EMS?
When would a core temp assessment be performed?
Who would perform this?
Does our school have a cold immersion tub
Where is it located?
Is it shaded?
Does it have everything needed to safely submerge and circulate my child?
Are our EAP’s and heat specific policy and procedures rehearsed and practiced with coaches and EMS?